ACQAs and the Quest for Real Value in Health Care
November 17, 2020It’s an exciting time in the health care industry. Yes, it can feel fragmented and hard to navigate, and yes, it’s always changing. So why is it exciting? Because that opens opportunities for innovation.
Like the large-scale movement toward value-based care and a provider compensation model focused on quality of outcomes as opposed to quantity of services.
But here’s the truth: Innovation doesn’t happen in a vacuum. Making positive change happen and work in the real world requires new ways of thinking, doing, partnering, and collaborating.
That means getting out of the office to visit practices and employers and bringing an open mind. It means collaborating on ways to bring the cost and quality sides together in ways that not only meet everyone’s needs but also exceed their expectations.
Innovation doesn’t happen in a vacuum. Making positive change happen and work in the real world requires new ways of thinking, doing, partnering, and collaborating.
The seeds were planted early
The emergence of Accountable Care Organizations (ACOs) in the early 2010s was the result of sweeping changes ushered in by the Affordable Care Act (ACA). There were new pressures on everyone across the entire system: providers, patients, and insurers. Questions emerged around who controlled care management and who was in charge of the patient care journey.
This was when Excellus BlueCross BlueShield began developing our own approach to value-based care, epitomized by our Accountable Cost and Quality Agreements (ACQAs, pronounced aquas).
If there is good alignment and collaboration, plans can spend more of their time and resources on appropriate investments that keep patients at the center of care.
This puts care management at the point of care members trust most: their doctors.
Nearly a decade in, the data tells us our strategy is working. So we wanted to share the critical elements that are key to helping a plan to improve quality, eliminate inefficiency, and lower costs advance from looking good on paper to achieving real-world success.
Putting patients at the center of care
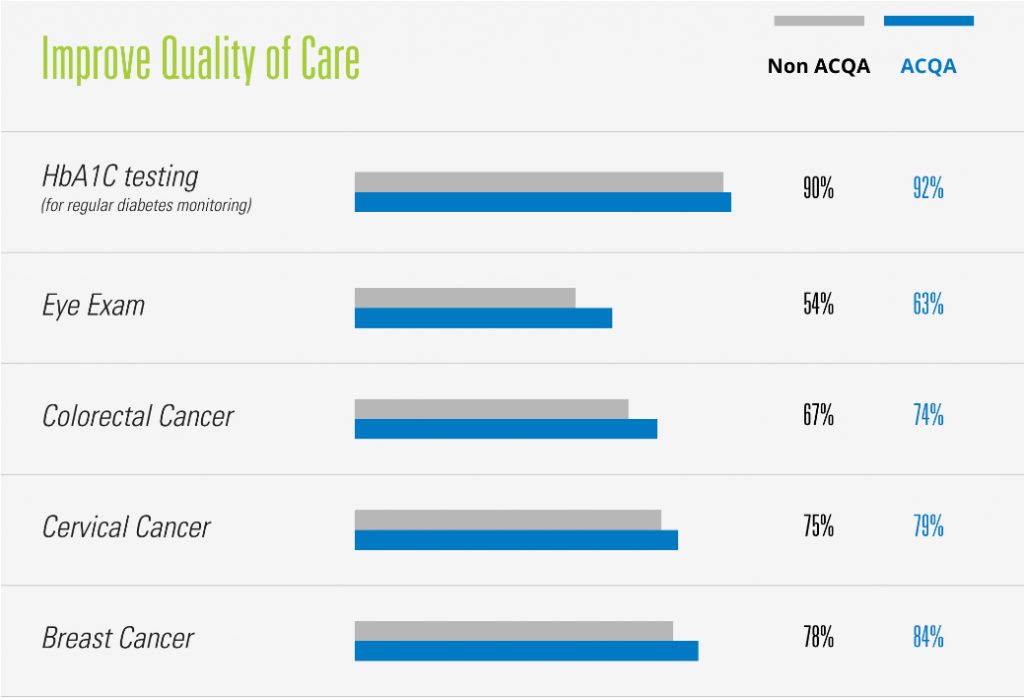
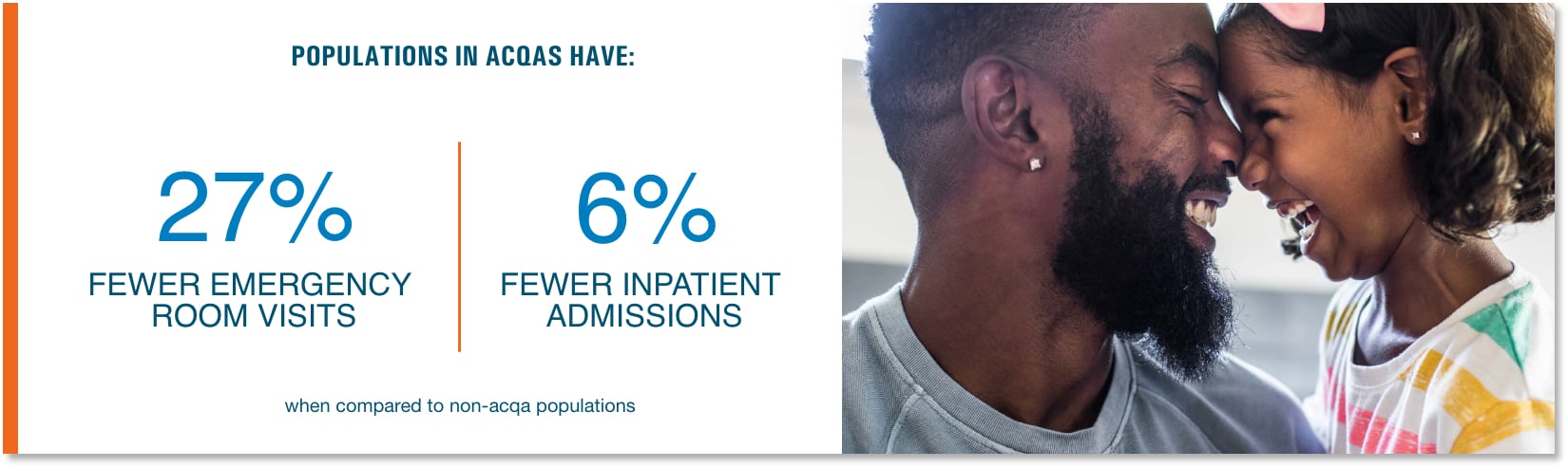
If you look at ACQA providers versus non-ACQA providers, you’ll see that preventive care visits and screening rates are higher across the board with ACQAs — proof that the investment is working.
When you can eliminate duplication of care and avoid unnecessary ER admissions because you’ve helped people stay healthy, you’re going to see real value.
This type of innovation and collaboration is important. The money we’re able to save gets funneled back into our communities and directly benefits local practices and community organizations. For example, we recently invested in retinal scopes to help a health system ensure their diabetic patients could have their eyes checked regularly.
More than just providing data and financial structure, we’re able to make tangible investments that help put in place measures that drive improvements.
A scientific and holistic view of data
The role of a health plan is only one piece of the puzzle. Providers have always had access to clinical data. Plans have always had access to claims data.
If a member was prescribed medication or had to visit an ER while on vacation, the primary care doctor would have no way of knowing unless the member told her.
No more. Our data aggregation tool brings clinical and claims data from diverse platforms together to extract actionable insights and quickly share them to help providers make the most informed decisions.
Providers can access this full data picture for all their patients, even those who aren’t Excellus BCBS members. They can check progress across all the quality measures. As a payor, we don’t see the data, but we feel good knowing we’re enabling providers to understand what’s going on systemically to better manage care for the entire population they’re accountable for.
If we’re scientific in how we use that information and data, we can help drive smarter decision-making to truly improve the health of the community and control costs by guiding patients to the most efficient and effective treatment.
The money we’re able to save gets funneled back into our communities and directly benefits local practices and community organizations.
Laying the infrastructure for the future
We’re remodeling the relationship that’s existed between health plans and providers for as long as health plans have been around. And we’ve seen enough promise and potential to date to know we’re on the right track.
This level of systemic and cultural change takes time. Building trust with providers takes time. But we knew this going in. We have the approach, long-term strategy, holistic perspective and commitment necessary to lead the value-based care movement for years to come.