A Balancing Act: Navigating the GLP-1 Trend
January 25, 2024Diabetes is one of the top trend drivers of pharmacy costs due to the growing diabetic population and newer, more expensive therapies recommended earlier in the treatment plan. Since 2006, medications like Ozempic® and Trulicity® have been used to treat Type 2 Diabetes. Today, they are gaining popularity as celebrities and social media influencers tout their weight loss benefits. As a health plan committed to providing access to high-quality and affordable health care, the rising trend of GLP-1 therapies demands careful consideration.
What is a GLP-1 medication?
These drugs mimic a naturally occurring hormone, glucagon-like peptide-1 (GLP-1), that plays a crucial role in regulating blood sugar levels.
GLP-1 helps slow stomach emptying and aids in decreasing appetite. It was known that these drugs often resulted in weight loss in addition to lowering blood sugar levels.
The first of these drugs approved specifically for weight management was Saxenda® in 2014. Two additional GLP-1s, Wegovy® and ZepboundTM, have been approved within the last two years.
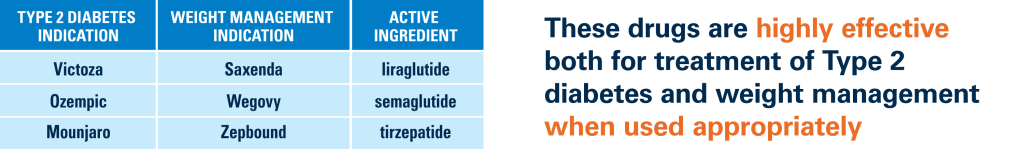
These drugs are highly effective both for treatment of Type 2 diabetes and weight management when used appropriately.
The problem arises when the diabetes drugs are prescribed off-label for weight loss, or the weight management drugs prescribed for cosmetic purposes in individuals who do not meet the Body Mass Index (BMI) requirements.
Unexpected demand and increased off-label prescribing has led to a shortage of these drugs at retail pharmacies, creating access barriers for diabetic patients. Additionally, with a price tag exceeding $1,000 per month, strategies must be in place to ensure the right member is receiving the right drug at the right time.
Our Approach
Excellus BlueCross BlueShield (BCBS) applies comprehensive utilization management strategies to ensure access to the most appropriate drug based on approved diagnosis and member characteristics.
These strategies include:
- prior authorization,
- step therapy, and
- quantity limits
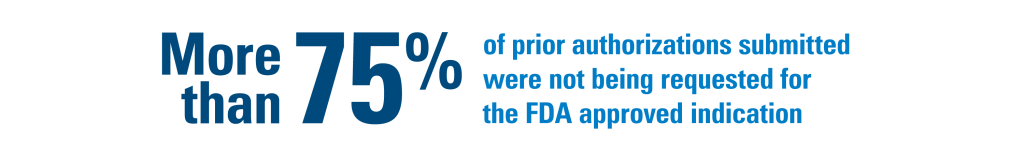
Our team of clinical pharmacists provide an unbiased review for each request of a GLP-1 to confirm medical necessity and safety. The same team created a strategy on the newest drug to treat diabetes, Mounjaro®, that has led to significantly less inappropriate and off-label use for weight loss. More than 75% of prior authorizations submitted were not being requested for the FDA approved indication. Employers can have confidence that their employees are protected against inappropriate prescribing and their healthcare dollars are protected against wasteful spending.
Our clinical team continuously monitors the market to quickly adapt to any changes.

In response to supply shortages of Wegovy®, Excellus BCBS has enhanced criteria for weight management policies.
When starting Wegovy®, the dose needs to be increased slowly to reach the effective dose for weight loss. Without lower strengths of the medication available in the marketplace, the dose titration cannot be completed reliably. Using the higher strengths without dose titration could put patients at risk for side effects. Any requests for members new to therapy are not being approved to ensure those that have started treatment continue to have access. Once the manufacturer can confirm supply will be restored, our strategy will be reassessed.
The trend in GLP-1 therapies requires the Health Plan to proactively engage in strategic initiatives. By promoting evidence-based prescribing, evaluating cost-effectiveness, ensuring equitable access, and staying informed in the market, Excellus BCBS can play a pivotal role in navigating the complexities of this growing trend while prioritizing member care.
To learn more about the complex world of weight management drugs, listen to a recent episode of The Community Check-In podcast “The Real Deal on Weight Loss Drugs”. Our Senior Director of Pharmacy Strategy and Policy, Nicole Dawley, provides valuable insights into the background of the obesity epidemic, the science behind these medications and the importance of integrating them into a comprehensive weight management program. Excellus BlueCross BlueShield – Community Check-In (chooseexcellus.com)