Breaking Down Barriers to Optimal Health Benefits Everybody
May 17, 2023The impact of barriers to care on employees and businesses
Health Equity. This concept has been studied since the early nineteenth century by people involved in public health, sociology, and political economics.1 It’s also near and dear to our mission as a local not-for-profit health plan in Upstate New York. But only recently has it started to gain a stronghold in mainstream culture and captured the attention of well-intentioned individuals and businesses alike. We’re all growing more and more aware of the health disparities that face people right here at home and across our country.
Health equity is achieved when every person has the opportunity to achieve their full health potential – where no one is disadvantaged from achieving this potential because of social position or other socially determined circumstances.
Health disparities can be defined as preventable differences in the burden of disease, injury, or violence, or in opportunities to achieve optimal health, that are experienced by socially disadvantaged racial, ethnic, LGBTQIA+, and other population groups and communities. In other words, there are factors largely beyond a person’s control that act as barriers to optimal health and health equity – meaning they make some people more susceptible to poor health outcomes.

We are working diligently, along with others in the health care and welfare community, to dismantle systemic structures that have supported a legacy of inequities that continue to negatively impact the health of Americans, especially people of color.
Eliminating the barriers to optimal health requires partnership between organizations to address racism and the impact of social determinants of health. The impact of these barriers extends beyond the just the individuals burdened by them, including businesses.

Understanding the barriers that employees face
Let’s take a minute to think about the diversity of employee populations.
Some have college degrees, others only high school diplomas or on-the-job skills training. One person might be the primary earner at home, while another has a partner contributing to the household income. And maybe they work one full-time job, or multiple part-time jobs to make ends meet. Some own a home in a quiet suburban town, while others might rent in an urban or rural neighborhood that has faced systemically low investment or divestment. How many own a car versus rely on public transportation, and how close do they live not only to work but to quality, affordable health care and food options? Who faces discrimination, hate and even violence on a daily basis due to where they live or how they identify? Many probably speak English as their first language, but there are some who don’t and will struggle to find a mental health provider who speaks their native language so they can adequately and easily express their nuanced needs and have them understood.
If we look at the populations within our local Excellus BCBS service area, we can see evidence of this right here at home. For example:
- 12% of the Rochester region and 8% of the Syracuse region’s populations are Black.2 Among other things, we know that Black Americans tend to have a lack of trust in the health care system and are less likely to have a primary care physician and receive preventive services, leading to poorer health outcomes.3
- At least 1 in 10 New Yorkers experience food insecurity, with food-insecure New Yorkers being twice as likely to report unsatisfactory health.4 In our service area, we have counties like Montgomery and St. Lawrence with more than 14% of people facing food insecurity.
- New York state has the second highest Asian American population in the U.S., with 30.9% of Asian Americans nationally not fluent in English.5 Language barriers can lead to delays in accurate diagnosis and gaps in care.6
- More than 842,000 people live in rural communities within our local Excellus BCBS service area.2 Rural residents face issues like physician/provider shortages and far distances to access services, limited access to healthy foods, and higher smoking rates than their urban counterparts.
And the list goes on.
Our members—and your employees—are diverse in where they live, their education and income levels, race, gender identity and sexual orientation, and more. All of which impacts their ultimate health outcomes in one way or another.
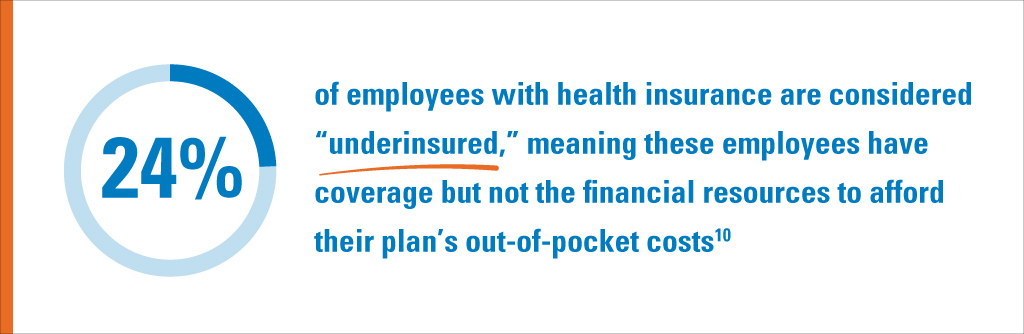
These barriers have an impact on not only their health, but also other aspects of their life, including work. They might miss work frequently due to things like lack of transportation, lack of safe, stable housing and childcare, unaddressed or poorly managed health needs, or caring for aging parents. When they are at work, their productivity might be lower with life concerns weighing on their mind. And financially, they’re facing excess out-of-pocket medical costs because they have put off getting the care they needed for too long.
It’s also important to recognize how removing one barrier might positively impact another part of a member’s life. For example, if you help a member, Mary, with access to transportation, she can now make it work reliably, make it to her doctors’ appointments, and can make it to the grocery store regularly. Mary’s life is positively impacted, her health is positively impacted, and her productivity at work is positively impacted.
Working towards greater health equity benefits everybody
At Excellus BCBS, health equity is threaded throughout our Synchronized Health approach to helping our members and groups see better outcomes, lower costs, and greater peace of mind. Our multidimensional health equity strategy centers around engaging, educating, and empowering our members, employer groups, and the community in order to break down these barriers to optimal health.
When we don’t have health equity, this costs everyone: members and their family, our health care system, and employers in terms of untapped productivity or excess medical costs. When we work together to address barriers and expand access to care in the community, members can see improvement in their daily lives, are more productive at work, and contribute more to their communities. This way, everybody benefits.
Resources you can use
- To learn more about what Excellus BCBS is doing to remove barriers for our members, download our Health Equity Brochure.
- Download our employer toolkit to learn how businesses can help promote health equity and empower members to seek help.
Sources:
2US Census Bureau
4https://nyhealthfoundation.org/wp-content/uploads/2023/01/NYHealth-survey-of-food-and-health.pdf
5U.S. Department of Health and Human Services Office of Minority Health, Accessed February 2023
6https://www.sciencedaily.com/releases/2011/01/110120151638.htm
7https://nam.edu/social-determinants-of-health-101-for-health-care-five-plus-five/
8Ani Turner, The Business Case For Racial Equity: A Strategy For Growth, Altarum/W. K. Kellogg Foundation, July 24, 2018.
9Ken Alltucker, “U.S. Doctor Shortage Worsens as Efforts to Recruit Black and Latino Doctors Stall,” USA Today, June 26, 2020.