How to Support Employees with High-Cost Conditions
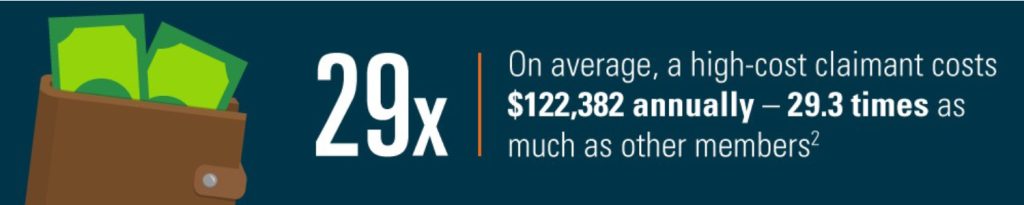
September 01, 2022Even though high-cost claimants represent only about 1% of members, they drive nearly a third of the health care costs for many employer health plans.1
These are usually members with chronic or complex conditions who are managing multiple health concerns at once. For them, the pressure can be overwhelming, leading to unexpected absences, loss of motivation, and changes to mood and personality. Not to mention, the health care costs can add up quickly.
To make sure your employees with high-cost medical conditions feel supported throughout their health care journey, it’s important to ensure your health plan has a proven strategy in place for connecting them with the resources they need.
Here are some things to look for in a strategy to help high-cost members achieve better outcomes, lower costs, and greater peace of mind.
Early identification for more proactive intervention
One of the first steps to helping members with high-cost conditions is to use data to identify them early enough for proactive intervention. For example, our High-Cost Claimant (HCC) Team at Excellus BlueCross BlueShield looks at a range of factors to identify at-risk individuals, including:
- Current year spend
- Risk factors
- Predictive analytics

The sooner high-cost members are identified, the sooner they can be educated on how to manage their conditions and prevent complications – and large claims – before they happen.
A dedicated team to keep employees engaged
Once a potential high-cost claimant has been identified, the next critical piece of the strategy is to ensure that support is being tailored to their unique needs. This could mean having a specialized care management team available to ensure they have the full range of care and support required to manage their conditions. For example, they might need guidance from a pharmacist, registered dietitian, behavioral health therapist, or many others, depending on the specific condition.
This specialized care management team can help members in a variety of different ways. They can help customize an outreach and engagement plan for members, educate them on the importance of following their doctor’s care plan, and help them adhere to it by encouraging follow-ups with their specialists. They can also assist members with interpreting their benefit package and claims history to identify potential solutions or ways to reduce costs.

Whether it’s connecting with the member’s doctors or delivering regular interventions via text, email, or phone calls, keeping members engaged with their care can deliver a range of benefits that will positively impact both their health and their overall cost of care, such as:
- Averting care away from acute care
- Reducing costly ER visits and preventable admissions and readmissions
- Helping individuals feel more confident in managing their conditions
Providing personalized care for those who need it most
Being there for employees through difficult circumstances is more than just the right thing to do; it lets your team know that you value them as people, and genuinely care about their wellbeing. And with the right strategic partner at your side, you can give them the support they need to live healthier, happier, and more productive lives.
Check out this infographic to see the results the Excellus BCBS High-Cost Claimant Team has been able to achieve.
Sources
1Blue Health Intelligence analysis of 2018 BCBS member claims data, 2020